Today we’d like to introduce you to Tessa Gittleman.
Hi Tessa, thanks for joining us today. We’d love for you to start by introducing yourself.
If you had asked me as a child what I wanted to be when I grew up, I would have told you, “anything but a therapist.” I had seen quite a few clinical specialists before I was even in high school. These providers labeled me with diagnoses that explained the symptoms I was experiencing, but no matter how many worksheets I did, how much validation they gave, or how many medications I tried, nothing seemed to make it better. I spent more than a decade of my life leaving therapy feeling worse than I did when I had arrived; like a failure, invalidated, and like I was crazy for wanting to trust what my body was telling me. Then, in my early 20’s, I learned that much of my mental illness was actually chronic illness I had my whole life, but had gone undiagnosed.
I discovered the chronic illness after a lifetime of career losses, mostly because my body could not sustain the work. My first love, restaurants, was learned from David Fhima, before I could even drive a car. By 17, as much as I loved restaurant life, I learned it didn’t love me. Dislocated fingers, tension headaches, and being forced to spend days on floor with my back being out after a shift, I knew I had to make the switch to from restaurants to food media. My boss for the following years, and mentor in this venture, was Andrew Zimmern (before and during his transition to his Food Network life). I loved it, except it also had an increasing and intense impact on my body—spontaneous allergic reactions to foods that had been historically safe. Yet again, I was forced to pivot, choosing advertising with hopes it would be all the things I love, but with none of the medical hazards. I had no such luck.
After a couple of years of being a professional patient in the Mayo health system, I finally had a set of diagnoses that helped my world make sense. The problem was, I was medically disqualified from most jobs, and if I wanted to work, it needed to be low impact, temperature controlled, hypoallergenic, and I would need to have flexibility and control over my schedule to be responsive to seasonal health challenges or ongoing medical care. It became clear that the only job I could do sustainably, with a cosign from my providers, was the one I thought I never would be: a therapist.
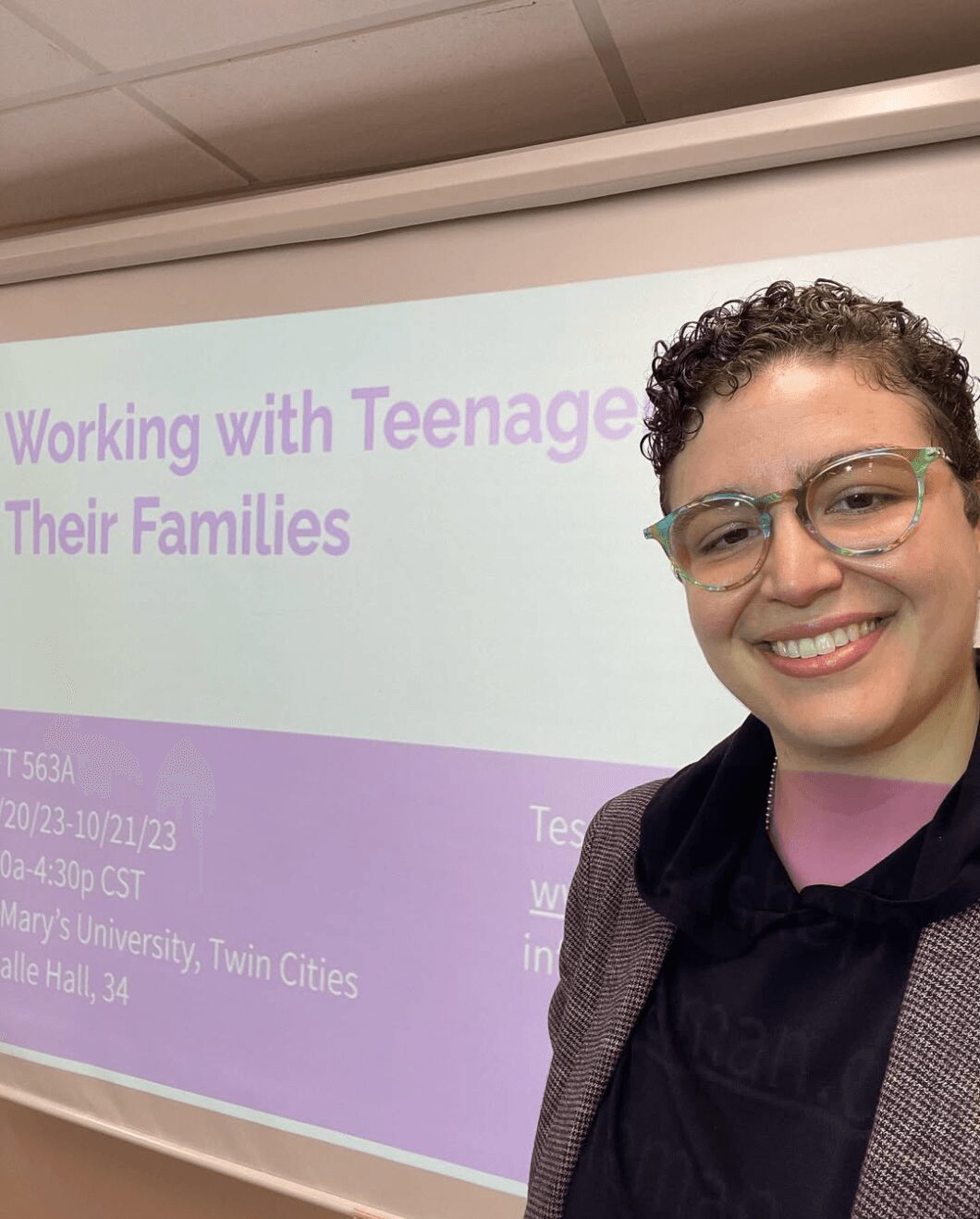
I decided to go to St. Mary’s University (Twin Cities) to pursue a Master’s degree in Marriage and Family Therapy degree; my idea of professional harm reduction was, if I had to do a job I never wanted to do, I wanted to be the kind I had never heard of before. As it turned out, I genuinely liked it. I had never had a therapist who could balance the needs of the individual with the needs of the system, the biological with the psychological and social, or talked about the process of things instead of just the outcomes. I felt very at home, settled, and at ease in this orientation to the work.
With my fresh optimism about the field, I started my practice working with kids, adolescents, and their families. I thought, like many therapists do, that I wanted to help at a time and in a way that I felt acutely failed by the adults around me. However, in doing that work, I learned that I loved working with their dads. Almost a decade later, my specialties evolved into: Obsessive-Compulsive Personality Disorder (which is distinct from OCD), Twice Exceptional Individuals (those with a high IQ and neurodivergence), and working with relational gaps, whether that be different generations, cultures, or neurotypes. I currently work for myself at a self-named practice in Golden Valley, MN, teach at St. Mary’s University in the Marriage and Family Therapy Master’s program, and am an AAMFT, MN BBHT and BMFT Approved Clinical Supervisor.
I’m sure it wasn’t obstacle-free, but would you say the journey has been fairly smooth so far?
Compared to what clinicians today face when entering the field, I have had a charmed path. Certainly there were bumps along the way… Ableist supervisors, clinics prioritizing profits over people, and shifting to tele-health during the COVID-19 pandemic, having never had experience with remote sessions, all stand out as some pain points. Perhaps the most difficult: No one warns you that, when you do this work full time, you don’t have the same capacity for the people in your life that you used to. Your social battery, patience, and boundaries all get renegotiated when you start caring professionally for people.
With that said, the last five years have undoubtedly been harder than the first five, and I say that with the incredible privileges of having a waiting list, working outside of the insurance model, and being my own boss. I cannot go more than a few days without hearing devastating, global and local news events from my clients. I have had too many supervision sessions where the clinician is at work, in an office full of clients and providers, as police knock about an active shooter in the area. Early in COVID, we all coped with stable ambiguity, but it’s evolved into a perpetual uncertainty that results in increasing rates of: ambivalence, moral injury, terminal loneliness, and hopeless for providers and clients alike.
As if that weren’t enough, clinicians have to stay up on rapidly changing policy shifts and arbitrary requirements to stay compliant. For my peers working at an insurance based practice, trying to make a living off the margins of low reimbursement rates (even lower for relational sessions, if they’re covered at all), practices are increasingly looking to be bought out by a hospital system or insurance company rather than go under. In my fourth year as a supervisor, I continue to watch waves of new graduates get the highest needs clients, and all of the resources we used to be able to offer, fewer and fewer exist. Consequently, more clinicians are leaving the filed before, or shortly after, licensure; they’re reducing their caseloads, retiring early, or otherwise trying to survive. It’s hard to continue to see that play out and, especially being a systemic therapist, feel helpless to stop it.
Thanks for sharing that. So, maybe next you can tell us a bit more about your business?
1. What should you know: For being a queer, chronically ill, Jewish woman working with predominantly cis-gendered, heteronormative, Christian men
1. More specifically:
1. My specialty: I am the foremost OCPD specialist in the state, and one of few in the world
2. My work outside of the office doing: Public speaking, clinical training, supervision, and teaching; I especially love presenting outside of the mental health space, such as offices and communities, on overcoming ambivalence, what “being relational” means, and how people can survive within broken systems.
3. My clinical orientation: I am a post-modern, experiential, systemic therapy that helps people overcome ambivalence and polarization in the world through practical, digestible, and sustainable ways clients continue to maintain without me. My therapy idols are Esther Perel and Carl Whittaker.
4. The services I offer:
1. In addition to individual, relationship, and family counseling in 60, 90, and 120 minute intervals…
2. I offer “Marathon” Intensives to families, teams, couples, and individuals, which range from 4-8hrs in a day, up to two days (because chipping away at things doesn’t always help)
3. Supervision, Continuing Education Trainings, and Professional consultation
4. Public speaking and professional writing
5. “Walk and Talk” therapy, for people who need a bit of movement to process
2. What sets me apart from others?
1. I believe that therapy is more effective when clients are able to explore and manage discomfort, which is why I aspire for clients to be 20% uncomfortable, and notify me if it exceeds that so we can course correct to a more sustainable discomfort.
2. I require all of my individual clients to bring in someone from their life, whom they can be in a positive or complicated relationship to, in order to get perspective on what’s changed every 3-6 months. This makes the work more objective, dimensional, and facilitates improved community support through more open dialogues.
3. I believe that clinical concepts need to be put into a common and familiar language for clients, which is why I often watch their favorite shows or learn about their industries; learning what they are already familiar with allows me to take something foreign and make it digestible for them.
4. I have had bad therapy and make efforts to ensure that clients never experienced the same hurt, disappointment, and invalidation that I experienced as a consumer.
3. What are you most proud of band wise?
1. Having never invested in advertising or branding, I feel really incredible with how many emails I get thanking me for my website… Specifically: the directness, authenticity, and transparency continues to resonate with people, even years later. I am always humbled, flattered, and appreciative of people who reach out because they feel like someone “gets it,” whatever “it” is.
4. What do you want readers to know?
1. The best indicator of outcomes for clients isn’t the therapist, their modality of choice, or whether or not homework gets done between sessions—the therapeutic relationship between provider and client is what facilitates change. If your therapist isn’t a good fit, it’s okay to try to find someone who might be.
2. No one has to choose between a traditional therapist and a therapist like me; they can have both! Lots of my clients have someone they meet with every week, using me more as a spot-check or coach focused on the bigger picture rather than short-term survival.
3. I am happy to do a free, 30-minute consultation to see if we’re a good fit. If we’re not, or I cannot get you in soon enough, I will be happy to refer you to people I like and trust.
If we knew you growing up, how would we have described you?
As a kid, I was described as precocious and an “old soul,” often preferring adults to people my own age until I was well into high school. As a young child, I couldn’t do the traditional things kids would do without injury, overwhelm, or debilitating boredom (sometimes all together). Minnesota summers tubing on the lake? Dislocated shoulder. Minnesota winters on the tow rope of a tubing hill? Dislocated shoulder. Playing dress-up with the girls? Allergic reaction. Play sports with the boys? Plural injuries…. It made staying at home safer, often preferring to make dinner for my family, do a chore, or read in my room.
Once I got to high school, I finally started to find “my people” who were interested in government, systems, and the world. I was on Student Council, tried the golf team (until even that became too much for my body), and continued to cook at home and in restaurants. College and graduate school also provided space for iterative improvement in my social capacity, connection to others, and ability to play. The friends I have and maintain since before becoming a therapist report that this is the most playful that they have ever known me to be, which I guess feels like an appropriate “Benjamin Button”-esque story arch for someone who was forced into being prematurely geriatric.
Pricing:
- Intake appointment: $350
- 60 minute session: $200
- 90 minute session: $300
- 120 minute session: $400
- Marathon session (min 4hrs): $1600 (base)
Contact Info:
- Website: https://www.tessagittleman.com
- Instagram: https://www.instagram.com/tessagittlemanlmft/
- Facebook: https://www.facebook.com/117147911384151/
- LinkedIn: https://www.linkedin.com/in/tessa-gittleman-2576621a2/
- Yelp: https://www.yelp.com/biz/tessa-gittleman-lmft-golden-valley
- Other: https://www.shor.by/tgittleman